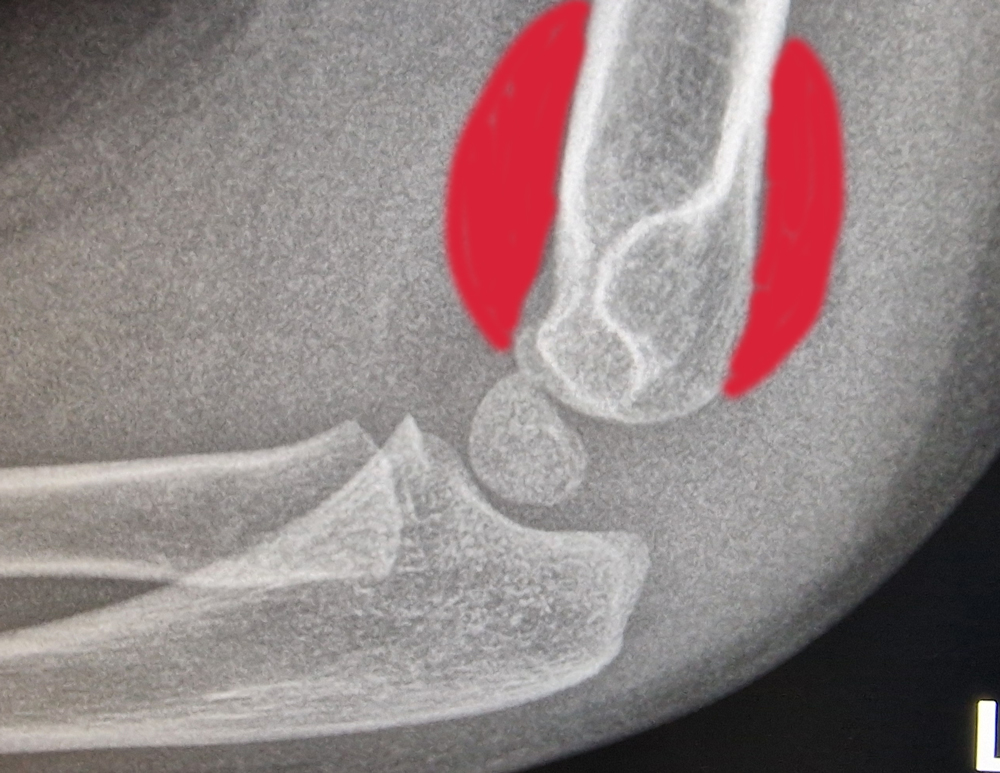
Fat Pad Sign – Ventral and Dorsal
IntroductionA supracondylar fracture is a type of break in the bone located just above the elbow joint (distal humerus). It is the most common type of elbow fracture in children, typically occurring between the ages of 5 and 7 years.
Anatomy
The distal humerus is the lower part of the upper arm bone, near the elbow. This area includes the humeral condyles, which articulate with the radius and ulna to form the elbow joint. Understanding the anatomy is crucial for recognizing the types and implications of supracondylar fractures.
Mechanism of Injury
Supracondylar fractures often occur due to a fall on an outstretched hand (FOOSH). This type of fall transfers a significant amount of force to the elbow, causing the distal humerus to break. These fractures are particularly common during activities like running, climbing, or playing on playground equipment.
Classification
Supracondylar fractures are classified based on the direction of the fracture line and the degree of displacement:
1. Extension Type (95%): The distal fragment is displaced posteriorly. This is the most common type.
2. Flexion Type (5%): The distal fragment is displaced anteriorly.
Additionally, fractures are classified by the Gartland system:
– Type I: Non-displaced fractures.
– Type II: Displaced fractures with an intact posterior cortex.
– Type III: Completely displaced fractures with no cortical contact.
Clinical Presentation
Children with a supracondylar fracture typically present with:
– Severe pain and swelling around the elbow.
– Visible deformity in the case of displaced fractures.
– Inability to move the elbow.
– Possible neurovascular compromise, indicated by decreased pulse, numbness, or tingling in the hand.
Diagnosis
Diagnosis is primarily based on:
– Clinical Examination: Assessing for deformity, swelling, and neurovascular status.
– Imaging: X-rays of the elbow in AP and lateral views are essential to confirm the fracture type and displacement. Occasionally, oblique views or a comparative view of the uninjured elbow may be required.
Treatment
The treatment approach depends on the type and severity of the fracture:
– Type I: Typically managed with immobilization in a splint or cast for 3-4 weeks.
– Type II and III: Often require closed reduction and percutaneous pinning (CRPP) to realign and stabilize the bone fragments. Severe cases might need open reduction and internal fixation (ORIF).
Complications
Potential complications include:
– Neurovascular Injury: Damage to the brachial artery or median nerve is a concern and must be assessed promptly.
– Compartment Syndrome: Increased pressure within the forearm muscles, leading to decreased blood flow and potential muscle and nerve damage.
– Malunion: Improper healing of the fracture can lead to deformity and functional impairment.
Recovery and Follow-Up
After initial treatment, regular follow-up appointments are essential to monitor healing through clinical exams and repeat X-rays.
-Physical therapy may be needed to restore full range of motion and strength in the elbow.
Prevention: Preventing supracondylar fractures involves ensuring safe play environments for children, using protective gear during sports, and educating parents and caregivers about fall prevention strategies.